Understanding Prostate Cancer
Prostate cancer is a significant health concern for men worldwide, particularly as they age. The prostate, a small gland located below the bladder, plays a role in producing seminal fluid. When cancerous cells develop in this gland, it can lead to a variety of symptoms such as difficulty urinating, blood in the urine, or pelvic discomfort. Understanding the nature of prostate cancer is crucial for early detection and treatment.
Statistics reveal that prostate cancer is one of the most common types of cancer among men. According to recent data, it ranks second in cancer-related deaths among men, following lung cancer. However, the prognosis for prostate cancer is generally favorable, especially when detected early. This makes regular screenings and awareness of symptoms essential for effective management.
Factors contributing to prostate cancer include age, family history, and ethnicity. Men over 50, those with a family history of prostate cancer, and African American men are at a higher risk. Lifestyle factors such as diet and physical activity also play a role, although their exact impact remains under research. Understanding these risk factors helps in making informed decisions about screening and preventive measures.
Diagnosis and Screening
Diagnosis of prostate cancer typically begins with screening tests. The most common are the prostate-specific antigen (PSA) test and the digital rectal exam (DRE). The PSA test measures the level of PSA in the blood, with higher levels suggesting the presence of cancer. However, elevated PSA levels can also result from other conditions like benign prostatic hyperplasia (BPH) or prostatitis.
While the PSA test is a valuable tool, it is not definitive. Thus, if PSA levels are elevated, further testing such as a biopsy may be recommended. During a biopsy, small samples of prostate tissue are taken for analysis. Imaging tests like MRI or CT scans may also be employed to assess the extent of cancer.
Screening guidelines vary, but many health organizations recommend discussions about prostate cancer screening with men starting at age 50, or earlier for those at higher risk. It is important for individuals to weigh the benefits and risks of screening with their healthcare provider, as early detection can significantly impact treatment options and outcomes.
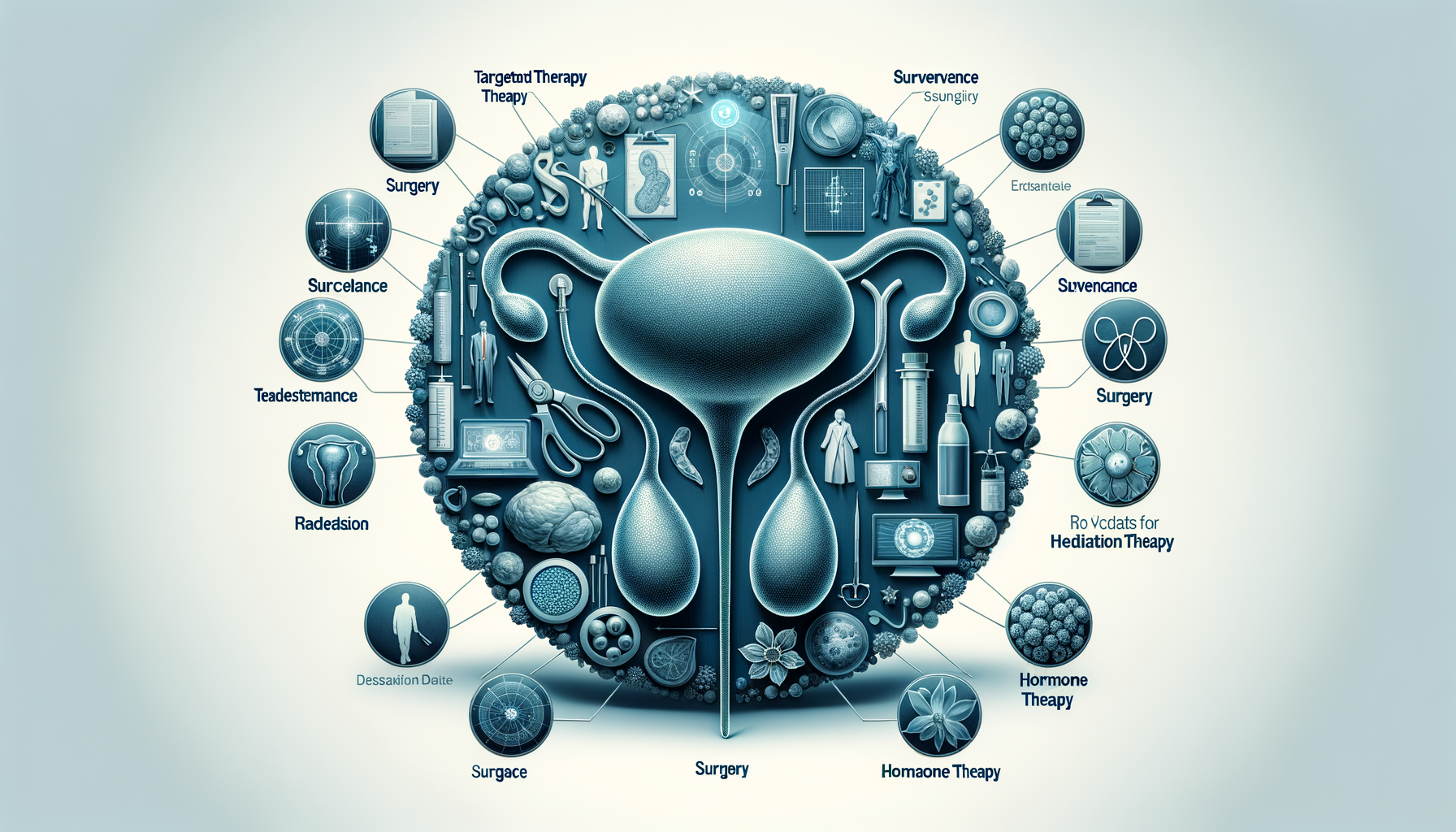
Treatment Options
Treatment for prostate cancer depends on several factors, including the stage of cancer, the patient’s age, and overall health. Common treatment options include active surveillance, surgery, radiation therapy, hormone therapy, and chemotherapy.
Active surveillance is often chosen for low-risk cancers, where the cancer is closely monitored for any changes. This approach avoids or delays the side effects of more aggressive treatments. Surgery, such as a prostatectomy, involves the removal of the prostate gland and is often recommended for localized cancer.
Radiation therapy uses high-energy rays to target and kill cancer cells. It can be external or internal (brachytherapy) and is an option for various stages of prostate cancer. Hormone therapy, which reduces or blocks the body’s production of testosterone, is used to slow the growth of cancer cells. Chemotherapy, while less common, is an option for advanced prostate cancer that has spread beyond the prostate.
Each treatment option has its potential benefits and side effects, and decisions should be made in consultation with healthcare professionals, considering the patient’s values and preferences.
Emerging Therapies and Research
Research in prostate cancer treatment is ongoing, with new therapies and approaches continually being developed. One promising area is immunotherapy, which aims to harness the body’s immune system to fight cancer cells. Although still in the experimental stages for prostate cancer, it has shown potential in other cancer types.
Another area of research is targeted therapy, which focuses on specific genetic changes in cancer cells. These therapies aim to attack cancer cells while sparing normal cells, potentially reducing side effects. Clinical trials are crucial for advancing these treatments and offer patients access to cutting-edge therapies.
Advancements in genetic testing and personalized medicine are also shaping the future of prostate cancer treatment. By understanding an individual’s genetic makeup, treatments can be tailored to improve efficacy and minimize side effects. Staying informed about these developments is important for patients and healthcare providers alike, as they hold the promise of more effective and personalized treatment options.
Living with Prostate Cancer
Living with prostate cancer involves not just managing the disease but also maintaining quality of life. Support from healthcare providers, family, and support groups can make a significant difference in coping with the physical and emotional challenges.
Many men continue to lead active lives during and after treatment. Lifestyle changes such as a balanced diet, regular exercise, and stress management can support overall well-being and may even improve treatment outcomes. Nutritionists and fitness experts can provide guidance tailored to individual needs.
Emotional support is equally important. Counseling or therapy can help address feelings of anxiety, depression, or fear. Support groups provide a platform for sharing experiences and advice, fostering a sense of community and understanding.
Prostate cancer is a journey that affects not just the individual but also their loved ones. Open communication and a strong support network are vital in navigating this journey, ensuring that life remains fulfilling and meaningful despite the challenges.


Leave a Reply